
October 10, 2025
Key Takeaways
-
Standing for extended periods of time puts extra force on the plantar fascia and metatarsal bones, precipitating plantar fasciitis, metatarsalgia and stress injuries. Select shoes with quality cushioning and arch support and ditch worn pairs to relieve pressure.
-
Muscle fatigue caused by long hours on your feet weakens support for the arch, increasing your risk of tendonitis and chronic pain. In addition, add daily calf stretches, toe curls, and short movement breaks to keep everything strong and flexible.
-
The lack of circulation due to static standing causes swelling, numbness and slow healing, especially when it’s cold. Keep your feet warm, shimmy your weight back and forth and wear compression socks to aid circulation.
-
Hard surfaces combined with work boots and winter footwear common in Edmonton act like mini trampolines, increasing impact, joint strain and slip risk. Employ cushioned insoles, anti-fatigue mats and supportive insulated shoes that feature a wide toe box.
-
Be on the lookout for danger signs like stabbing heel pain, chronic throbbing, tingling, or noticeable swelling that can indicate ailments requiring attention. Know your symptoms, ice when necessary, elevate feet, and switch shoes to avoid flare-up.
-
If pain persists or significantly limits activity, see a professional for precise diagnosis and focused treatment. Learn about orthotics, physiotherapy, and custom prevention plans to combat standing foot pain.
Foot pain standing Edmonton refers to discomfort in the feet that occurs during long periods of standing among people in Edmonton, Alberta. Typical culprits are plantar fasciitis, flat feet, bunions, and abuse from hard floors. Cold winters can stiffen joints, and work in retail, health care, and oil and gas frequently translates to hours on the floor. Symptoms can vary from a mild heel or arch ache to a stabbing pain at the ball of the foot. Relief tends to be found in cushioned insoles, supportive shoes, and short breaks. Ice, gentle calf and arch stretches, and low-impact activity assist in many cases. For recurring pain, area clinics and physiotherapists provide evaluation, gait analyses, and personalized orthotics.
Why Standing Causes Foot Pain
Standing for long periods burdens the plantar fascia and other soft tissues, slows circulation when you’re still, and introduces accumulative stress that compounds throughout the day. Unsupportive or ill-fitting shoes magnify these forces and can convert short-term aches into long-term maladies.
1. Constant Pressure
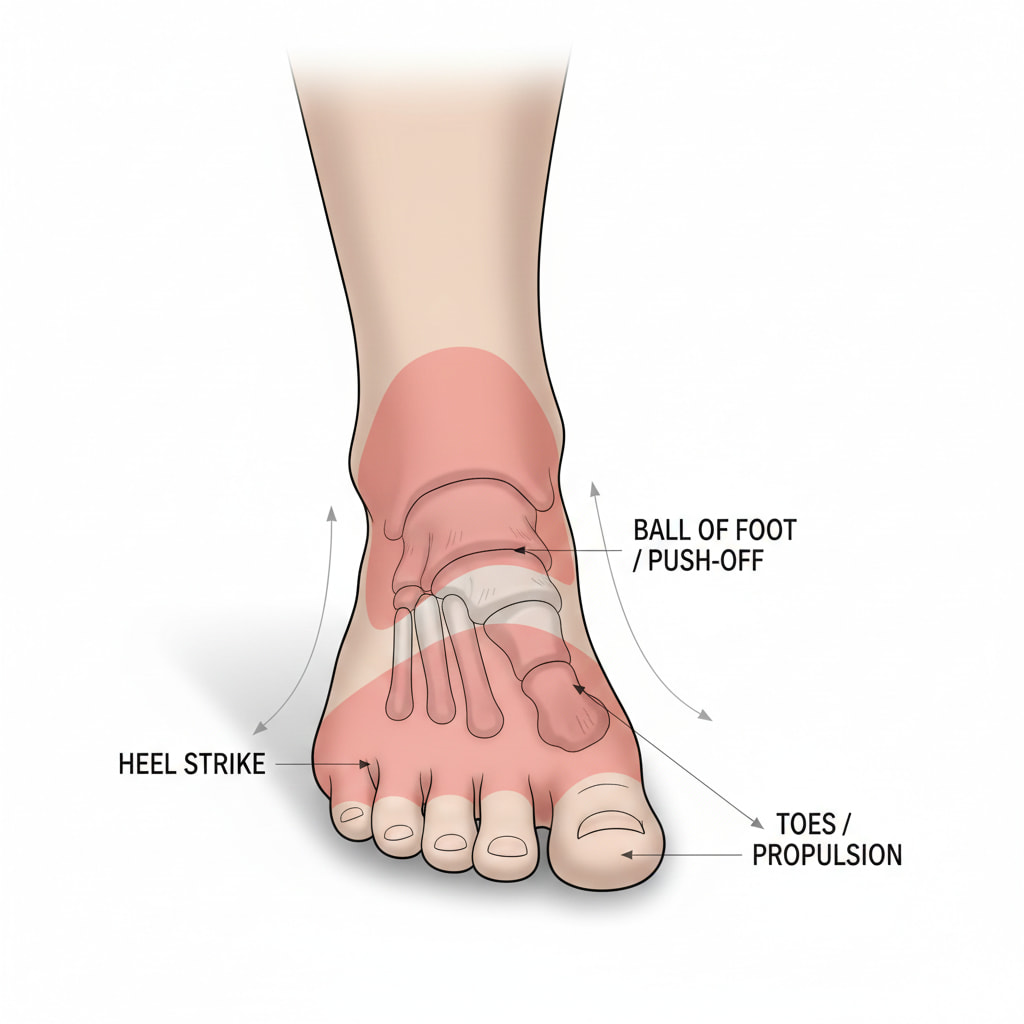 Non-stop pounding on the heels and the ball of the foot inflames the plantar fascia and the metatarsal heads. This frequently manifests as stabbing heel pain in the morning or a pebble-in-the-shoe sensation under the forefoot, typical with metatarsalgia. Swelling from too many hours on your feet can make pain surge quickly when you stand still.
Non-stop pounding on the heels and the ball of the foot inflames the plantar fascia and the metatarsal heads. This frequently manifests as stabbing heel pain in the morning or a pebble-in-the-shoe sensation under the forefoot, typical with metatarsalgia. Swelling from too many hours on your feet can make pain surge quickly when you stand still.
When pressure remains elevated, bones and soft tissue tire. That can lay the groundwork for metatarsal stress fractures and microtears in fascia or fat pads, particularly after high-impact sport or long work shifts.
Shoes with thin soles, hard insoles or tight toe boxes amplify this focal pressure. Poor fit fuels toe pain when you stand and can impinge nerves.
Table: Pressure points → Common problems
-
Heel → Plantar fasciitis, fat pad soreness
-
Ball of foot → Metatarsalgia, stress fractures
-
Toes → Nerve irritation, corns, joint pain
2. Muscle Fatigue
As foot and calf muscles become fatigued, they lose strength and finesse. Arch support drops, balance wavers, and minor missteps replicate with each step, increasing injury risk.
Chronic fatigue tugs on ligaments and tendons, including the Achilles, and eventually causes tendonitis and persistent lower-limb pain. Most experience a steady, achy accumulation in feet and calves that becomes more pronounced by evening.
Daily exercises:
-
Calf stretch (knee straight/bent), 30–45 seconds.
-
Plantar fascia stretch with towel.
-
Foot doming, short-foot holds.
-
Heel raises and seated calf raises.
-
Ankle pumps and alphabet.
3. Reduced Blood Flow
Standing still restricts the calf muscle pump. Blood flow reduces, fluid collects, and swelling abounds, leading to numbness, constricting footwear, and pulsing pain.
Recovery from these little strains lags when blood flow is low, so daily wear and tear from standing can turn into chronic pain. Cold weather constricts vessels even more and can exacerbate symptoms outside or in cold worksites.
Ways to boost flow:
-
Walk or shift weight every 20–30 minutes.
-
Ankle pumps, toe raises, and mini-squats.
-
Warm layers and dry socks in cold settings.
-
Compression socks (15–20 mmHg), if appropriate.
-
Elevate feet during breaks.
4. Joint Strain
Prolonged standing loads the ankle, sub-talar joint, midfoot, and toe joints. Stiffness and pain ensue and with time, this can accelerate arthritis changes, toe deformities, and joint instability. Overuse further increases the risk of sprains, ligament damage, and tendon tears, particularly when the ground is hard and your shoes are unsupportive.
Chart: Joints → Conditions
-
Ankle → Sprains, early arthritis
-
Subtalar → Instability, sinus tarsi pain
-
Midfoot → Joint strain, collapse
-
Toes (MTP) → Metatarsalgia, capsulitis
5. Arch Collapse
Additional pressure can pull the plantar fascia and tire arch support. Flat feet or bad insoles transfer load to the metatarsals, spur heel pain, and change gait. Plantar fasciitis often flares in the morning and after standing, while Achilles inflammation can ache along the back of the leg near the heel.
Signs and orthotics:
-
Signs: Tired arches, inward ankle roll, forefoot burn, shoe wear on the inside edge.
-
Orthotics provide firm arch support with a heel cup, a metatarsal pad for forefoot pain, and a shock-absorbing top cover for long standing.
Common Resulting Conditions
Standing for hours at a time can put strain on your feet and ankles, resulting in plantar fasciitis, metatarsalgia, bunions, and Achilles tendonitis. Unaddressed pain can blossom into chronic issues that make work and daily activities impossible. As with anything, early diagnosis and proper care minimize complications and decrease the risk of future damage.
|
Symptom |
Likely Condition |
|---|---|
|
First-step heel pain in the morning |
Plantar fasciitis |
|
Burning pain in the ball of the foot |
Metatarsalgia |
|
Pain and swelling at big toe joint |
Bunions |
|
Aching at back of heel with activity |
Achilles tendinitis |
Plantar Fasciitis
Plantar fasciitis is inflammation of the plantar fascia, the thick band that connects the calcaneus to the toes. It leads to stabbing heel pain on standing, exacerbated by the initial steps after rest or prolonged sitting. A lot of them experience pain along the arch. If heel pain doesn’t subside after a week of rest, ice, and over-the-counter pain meds, more specific treatment may be required.
Treatment frequently includes daily calf and plantar fascia stretches, arch-supporting orthotics, and physiotherapy loading and gait work. Flexing the foot up and down can relieve tightness in the fascia and Achilles. It can take months to recover, so consistent habits and the right shoes with a firm midsole and arch support make a difference.
Achilles Tendinitis
Achilles tendinitis is irritation of the tendon at the rear of the ankle. Repetitive standing, hard floors, and bad shoes increase the load on your calf and tendon, increasing your chance of injury. Left unchecked, it can lead to chronic pain or partial tears.
Relief comes from calf stretches, slow strengthening, heel-lift inserts, and physiotherapy techniques like eccentric loading and soft-tissue work.
Bunions
Bunions are bony bumps at the base of the big toes from joint strain and snug shoes. Hours of standing in narrow or high-heeled shoes accelerate pain and deformity and can cause arthritis, corns, or gait restrictions.
Select shoes that have a wide toe box, a stable sole, and a low heel. If pain continues, consider bunion treatments like splints, padding, custom orthotics, or surgical consultation.
Metatarsalgia
Metatarsalgia is pain and inflammation under the metatarsal heads, usually from increased pressure in the ball of the foot.
Reasons consist of thin-soled footsteps, high-impact work, and inadequate padding on difficult flooring. Rest, orthotics with met pads, and physical therapy assist in alleviating stress and enhancing push-off.
-
Symptoms: Burning forefoot pain, worse with standing. Numb toes. Stone-bruised feeling.
-
Prevention tips for workers: cushioned insoles, rotate tasks and breaks, choose shoes with a 10 to 15 millimeter drop, add shock-absorbing mats, keep body mass in a healthy range.
Edmonton's Unique Challenges
Edmonton’s weather, office environments and city shape exert a special kind of strain on feet. Edmonton’s long winters, heavy gear and hard floors are a recipe for overuse and acute injuries. Local foot care has to keep pace with these factors. A straightforward list keeps tabs on hazards associated with season, occupation, commute and surface.
Cold Weather Impact

Cold restricts blood circulation in the feet, thereby increasing numbness, impeding tissue recovery, and causing joints to feel stiff. When experiencing drops, we slip in our estimation of where to place our feet on ice or stairs and pile tissues in inconvenient locations. Winter’s short days reduce outdoor activity, which gradually saps foot and calf strength.
A lot of winter boots are stiff with minimal forefoot flex and minimal arch shaping. That rigid shell can transfer load to the heel or big toe joint and pinch wider feet when socks are bulky. On those long commutes through blizzards and freezes, this accumulates.
Icy sidewalks and parking lots breed slips, ankle sprains and forefoot bruises. Heatwaves and sudden thaws cause melt-refreeze cycles that maintain hazards at elevated levels throughout the season. For warmth and stability, insulate yourself with boots boasting firm heel counters, midfoot support and grippy soles. Layer thin wicking socks underneath a wool pair so your skin stays dry and warm without the bulk that distorts fit.
Heavy Work Boots
Heavy boots prevent the natural roll of the foot and the spring of the arch, which can fatigue small foot muscles and stress ankles and knees. In the oil, gas and construction type roles typical here, 12 to 16 hour shifts on sites or in plants exacerbate this.
Bad cushioning, narrow toe boxes, and inconsistent sizing cause corns, bunions, and perennial heel pain. Pick boots with strong arch support, shock-absorbing midsoles, and adequate forefoot width. Flip pairs to air out liners and foam to puff. Put hard or semi-hard inserts in when arches collapse due to load.
Hard Urban Surfaces
Standing and walking all day on concrete adds impact to feet, ankles, and knees. Transit hubs, warehouses, hospitals, and retail floors remain pressure points as the city grows quickly and sprawls.
Too hard floors connect to plantar fasciitis, metatarsalgia and stress fractures. With peerless homelessness rates, they increase risks from bare feet and extended pavement hours. Use shock-absorbing insoles rated for your body weight and install anti-fatigue mats at stationary work locations.
Best practices:
-
Mix sitting and standing in 20–40 minute blocks
-
Swap shoes midday to change pressure points
-
Keep stride short on slick routes during blizzards
-
Track pain zones weekly; adjust insoles or tasks
Listen to Your Feet
They’re early warning signs. Page 236: Keep tabs on little transitions from too many hours on your feet—numb areas, zings, sharp pokes, stabbing aches, or puffiness. Record what you wore, surface type, shift length and breaks. A quick symptom diary and straightforward checklist keep patterns clear. Balance checks help too: stand on one foot for 10 to 15 seconds or walk heel to toe in a straight line. Trouble here can indicate foot problems that increase fall risk, particularly for seniors.
Numbness or Tingling
Numbness or pins and needles usually indicate nerve squeeze or bad circulation. It may originate from snug shoes, laces that squeeze the top of the foot, or simply standing for extended periods.
If it persists, it can connect to nerve damage or underlying conditions requiring treatment. Act fast: loosen footwear, choose wider toe boxes, and swap to cushioned insoles. Take short walking breaks every 45 to 60 minutes to boost circulation.
Quick list: Causes include tight shoes, flat insoles, hard floors, cold temperatures, or swollen feet. Relief steps: Sit and elevate for 10 minutes, ankle pumps, calf raises, warm socks, and check socks that do not constrict.
Sharp Heel Pain
A stabbing pain beneath the heel frequently indicates plantar fasciitis. Pain at the back of the heel may indicate Achilles tendinitis or a heel spur. It likes to spike with morning or post-prolonged-standing first steps.
Treat with ice for 10 to 15 minutes, gentle calf and plantar fascia stretches, and supportive shoes with firm heel counters. Track pain on a scale from 0 to 10, the time of day, and triggers to determine if modifications assist and when to seek treatment.
Persistent Aching
A persistent, nagging pain means overuse or that it’s some kind of chronic beast that erodes mobility. Dismissing it can alter your gait and put additional strain on knees or hips and increase fall risk in seniors.
Alternate standing and sitting, use anti-fatigue mats, and do short stretch sets: toe curls, ankle circles, and wall calf stretches. Low-impact work, such as brisk walks, water aerobics, and tai chi, softens stiffness and strengthens feet and ankles.
At work: Rotate tasks, pace during calls, schedule 5-minute off-feet breaks each hour and log shoe wear time to know when to replace.
Visible Swelling
Swelling in feet or ankles indicates inflammation, sprains or sluggish circulation. It can re-ignite with prolonged static standing or constrictive shoes.
Try to raise your feet above your heart, apply cold packs, and wear moderately tight compression socks. Keep shoes supportive and socks warm to help flow.
Track side (L/R), time and activity links. About: Listen to Your Feet. Keep nails trimmed, skin moisturized, and wash and dry daily to slash fungal risk. As we age, thinner foot fat pads provide less cushion. Quality shoes and insoles assist in shock absorption.
Proactive Prevention Strategies
Nip foot pain from long hours on your feet in the bud with savvy equipment, consistent motion, and mini habits. The sooner you act, the better you will recover and avoid long-term pain.
Choose Proper Footwear

Choose shoes that have rigid heel counters, midfoot support, and surface-matched cushioning. A wide toe box prevents pressure on your forefoot and nails. For hard floors, seek out thicker midsoles. For wet areas, slip-resistant outsoles promote stability.
Schedule shoe replacement. As a general guideline, rotate running shoes every six to nine months or 400 to 800 miles. Look for midsole creases, canted heels, or scarred tread; these are indicators that the support is lost.
Pair shoes with the job. Safety boots for construction sites, orthopedic clogs for hospitals, and low-heel dress shoes for cubicles. Have a pair to rotate and let foam rebound.
Top features checklist: stable heel cup, arch support, shock-absorbing midsole made of EVA or PU, wide toe box, breathable upper, slip-resistant outsole, removable insole, and a light balanced weight.
Use Supportive Inserts
Orthotics and cushioned insoles distribute load throughout the foot, relieve pressure points, and direct alignment. This decreases tension on the plantar fascia and metatarsal stress.
Custom inserts can address flat feet, plantar fasciitis, metatarsalgia and overpronation. Off-the-shelf options work for many, but custom devices meet complicated demands.
Tuck some inserts into work boots and daily shoes to maintain support throughout the week.
Types and benefits include cushioned gel for shock, semi-stiff arch for control, metatarsal pads for forefoot load, heel cups for fat-pad preservation, and heat-moldable insoles for customized comfort.
Stretch and Move
These short, regular breaks protect tissues and accelerate healing over the long term. Calf and Achilles stretches can reduce healing time and may help prevent recurrent injuries.
Include toe/heel raises, towel scrunches, ankle circles, toe curls, ankle alphabets. Try for 5 to 10 minutes, twice daily. Keep your weight in check to reduce stress on the plantar ligament. Make sure to keep your feet clean and dry, and that nails are trimmed straight to avoid pain and infection. Physiotherapy combines training, stretches, and braces for immediate relief and sustainable outcomes.
Table—quick routine: standing calf stretch (30 to 45 seconds, 2 to 3 sets per leg); wall Achilles stretch (20 to 30 seconds); ankle circles (10 each way); toe curls with towel (10 to 15 reps); seated foot roll on a ball (1 to 2 minutes). Knowledge and drills fortify your body with strength, elasticity, and free movement and forestall pain down the road.
Modify Your Workspace
Place anti-fatigue mats on hard floors. They reduce peak pressure and calf load.
Alternate activities to alternate standing and sitting when possible. Schedule timers for quick walks to get the blood flowing. Periodically prop one foot on a 10 to 15 cm footrest to unload the lumbar spine and forefoot.
Workspace checklist: anti-fatigue mat, height-adjustable bench, footrest, stool for task rotation, reachable tools to limit twisting, supportive floor-safe shoes, and clear space to move.
When to Seek Professional Help
Standing foot pain that does not ease with rest, ice, or simple shoe tinkering requires a more detailed examination. Timely care can prevent small issues from becoming chronic problems at work, home, or sport.
Ongoing or intense pain should be evaluated by an experienced podiatrist or foot specialist. If pain persists for weeks with no obvious improvements, it may indicate plantar fasciitis, stress fractures, nerve entrapment, or joint wear that requires targeted treatment. Pain that impedes daily activities such as standing through a shift, walking 1 to 2 kilometers, or climbing stairs typically fares better with focused treatment than additional rest. Difficulty bearing weight, limping, or waking at night from foot pain are red flags that warrant immediate evaluation.
This is where professional help plays a crucial role, as accurate diagnosis is key. A clean exam and, when necessary, imaging separate soft tissue strain from bone or nerve problems. This is important because the correct treatment plan for heel pain caused by fascia strain is different than for a stress fracture or tendinopathy. Warning signs include swelling, warmth or redness that won’t subside, deformities such as a bunion that displaces the big toe, stiffness in the ankle or midfoot that reduces range of motion, or pain radiating up the leg or into the back. These indicate joint, tendon or nerve issues that could spiral without attention. According to the diabetic foot specialist, those with diabetes or chronic foot problems should schedule routine screenings to detect skin risk, pressure zones, and nerve damage as soon as possible.
In Edmonton, Edmonton Foot Clinic provides comprehensive foot pain treatment for standing-related strain. Services include custom orthotics to improve load and support, footwear advice for long hours on hard floors, and physiotherapy that builds calf strength, improves ankle range, and guides safe load progress. Advanced therapies, such as shockwave for stubborn plantar fasciitis or tendon pain, taping to offload sore tissue, and targeted injections when indicated can speed healing. For example, a retail worker with heel pain may pair orthotics with calf loading and shockwave, while a chef with forefoot pain may use metatarsal pads, shoe changes, and mobility work. Booking a foot care appointment at Edmonton Foot Clinic gives a full assessment, a clear plan, and ongoing follow-up to track gains and adjust care as you get back to pain-free standing.
Conclusion
Long days on your feet can take a toll on even the sturdiest feet. Hard floors, tight shifts, and Edmonton’s cold snaps only add more strain. Little treads pile up quick. Change out worn insoles. Rotate shoes with stiff heel hold. Take little sit breaks. Stretch your calves and arches for 60 seconds. Map pain by time and location, such as heel, arch, or ball. Basic notes aid in identifying trends.
Real red flags need attention. Heel stab with the first step. Numb toes post shift. Swell that sticks around more than a day. Pain that wakes you up at night. See a foot pro in Edmonton for an exam and plan. Inquire about gait checks and shoe fitting.
Need actionable next steps? Post your sore spot, standing hours, and style of shoe. Let’s plot a solution.
Frequently Asked Questions
Why do my feet hurt after standing for long hours?
Standing places continual stress on your arches, heels, and forefoot. Muscles tire, ligaments strain, and joints compress. Hard floors and sappy shoes raise stress. Over time, this can lead to inflammation and pain.
What foot conditions are common from prolonged standing?
Common foot problems are plantar fasciitis, heel spurs, Achilles tendinopathy, metatarsalgia, bunions, and neuromas. You can observe flat feet symptoms intensify. Early treatment keeps it from becoming chronic.
Does Edmonton’s climate make foot pain worse?
Cold, dry winters tend to stiffen muscles and tendons. Ice and snow alter your gait and increase impact. Seasonal shoes can have lousy support. This can intensify standing foot pain.
How can I prevent foot pain if I stand all day?
Wear supportive shoes with solid midsoles. Buy custom or good quality insoles. Throw down some anti-fatigue floor mats. Take micro-breaks to stretch calves and arches. Mix up your posture and shift weight frequently.
When should I see a foot specialist?
Consult if pain persists for more than two weeks, reduces activity, or includes swelling, numbness, or morning heel pain. Sudden sharp pain requires immediate attention. Early evaluation hastens recuperation.
Are insoles and orthotics worth it for standing jobs?
Yes. They increase arch support, straighten your foot, and relieve pressure points. Most people experience less pain and fatigue. Pick choices suited to your foot and activity.
What quick relief can I try at home?
Rest, elevate, and ice for 10 to 15 minutes. Apply light calf and plantar fascia stretches. Change to supportive footwear. Consider over-the-counter pain relief if applicable. If pain continues, seek an expert opinion.
Need more information? Check out the full range of services offered at our Edmonton foot clinic.
Here are other additional resources:
Canadian Centre for Occupational Health and Safety (CCOHS)
When To See a Doctor When You Are in Pain

